An all-in-one advanced EHR that keeps visits moving. Book a demo.

-
Solutions
-
Advanced EHR AI-powered, seamless workflows, improved patient care.
-
Practice Management Manage appointments and schedules efficiently.
-
Patient Engagement Enhance satisfaction with patient communication tools.
-
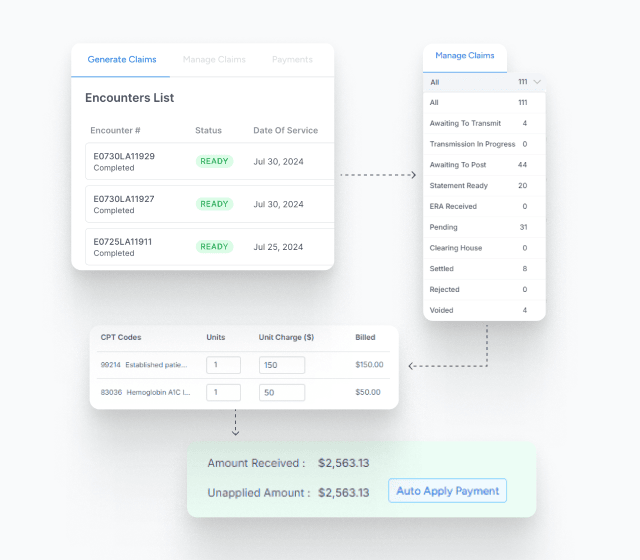
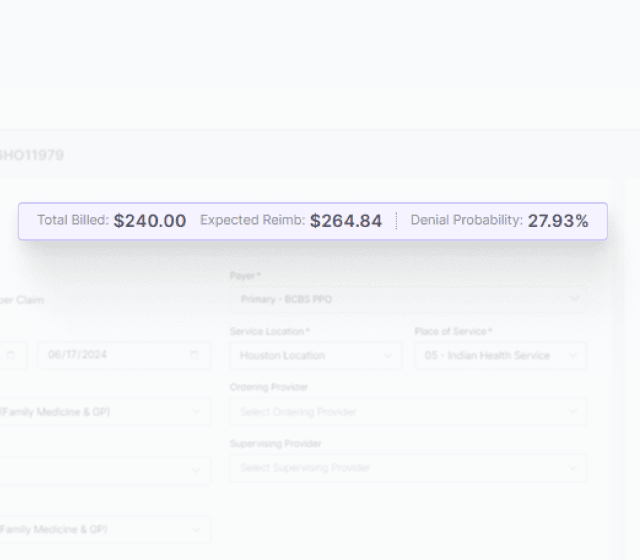
Billing and Revenue Cycle Management Streamline billing and boost revenue efficiency.
-
Analytics and Reporting AI analytics provide in-depth, interactive insights.
-
- Pricing
- Contact Us
- Resources










 No credit card required
No credit card required
 No Annual Commitment
No Annual Commitment